Itching or Discharge Down There? It Could Be a Vaginal Infection
- Duly Care
- Jun 18
- 8 min read
Vaginal infections are a significant yet often misunderstood health concern for women, cutting across age, geography, and lifestyle. They are more than just a source of physical discomfort. They can impact emotional well-being, relationships, and even self-confidence.
In this blog, you will learn about the types, causes, symptoms, diagnostic methods, treatment options, and prevention strategies of vaginal infections. Along the way, we'll address common myths and provide practical tips for protecting your vaginal health.
Key Takeaways
Vaginal infections occur due to disruptions in the natural vaginal flora or external factors.
Symptoms such as itching, unusual discharge, and discomfort during urination or intercourse are common.
Diagnosing and treating infections early can prevent long-term complications.
Preventive measures include practising good hygiene, safe sex, and maintaining a healthy lifestyle.
What Is a Vaginal Infection?

A vaginal infection, or vaginitis, refers to any condition that disturbs the natural environment of the vagina. The vaginal ecosystem is home to beneficial bacteria, primarily lactobacilli, which maintain an acidic pH of about 3.8 to 4.5, keeping harmful organisms in check. Harmful bacteria or yeast can overgrow when this balance is disrupted, leading to infections.
Common Types of Vaginal Infections
Bacterial Vaginosis (BV): Caused by an overgrowth of harmful bacteria, BV is characterised by a fishy odour, thin grey or white discharge, and itching. It is not a sexually transmitted infection (STI), but sexual activity can alter the vaginal microbiome and trigger BV.
Candidiasis: This yeast infections occur when Candida, a type of fungus, multiplies excessively. Common symptoms include thick, white discharge (often described as cottage cheese-like), intense itching, and redness.
Sexually Transmitted Infections (STIs): Certain infections like trichomoniasis, chlamydia, or gonorrhea can cause vaginal irritation and discharge. STIs are transmitted through sexual contact and often require immediate medical attention.
Non-Infectious Vaginitis: Allergic reactions to products like soaps, detergents, or sanitary products can cause non-infectious vaginitis, leading to irritation and discomfort.
Causes of Vaginal Infections
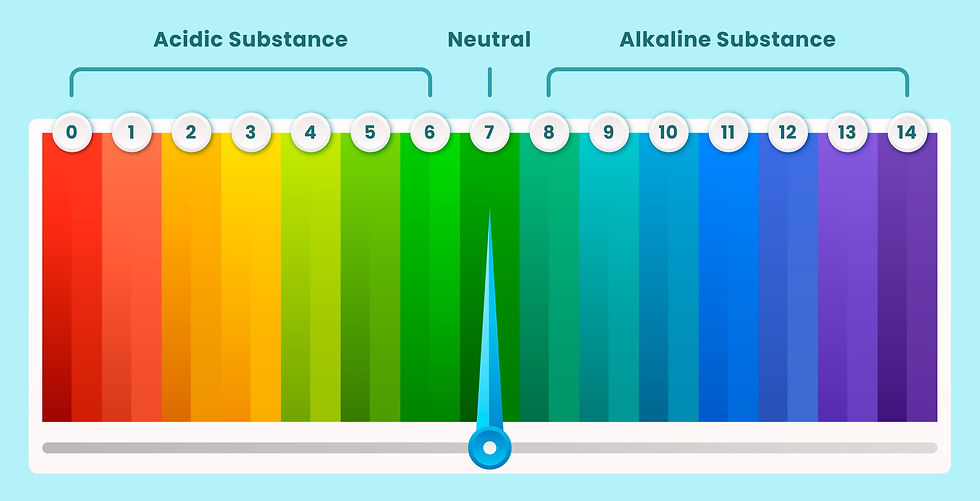
Vaginal infections result from a variety of factors, most of which disturb the delicate balance of the vaginal microbiome. The vaginal environment is naturally acidic, with a pH level between 3.8 and 4.5, maintained by healthy bacteria, primarily Lactobacillus. This balance ensures that harmful bacteria and yeast are kept under control. When disrupted, infections can occur.
Here are the primary causes of vaginal infections:
Imbalance in Vaginal Flora
The vaginal microbiome can be easily disturbed by factors such as antibiotic use, poor hygiene, or hormonal changes. Antibiotics, for instance, not only kill harmful bacteria but also the good bacteria that maintain a healthy balance. This can lead to an overgrowth of harmful bacteria (Gardnerella vaginalis) or yeast (Candida albicans), resulting in bacterial vaginosis (BV) or yeast infections, respectively.
Hormonal Changes
Hormones play a crucial role in maintaining vaginal health. Estrogen helps to maintain the thickness of the vaginal walls and supports the growth of healthy bacteria. Any fluctuation in estrogen levels - whether due to pregnancy, menstruation, menopause, or hormonal medication - can alter the vaginal pH, making it less acidic and more hospitable to infections. For example, menopause often leads to thinning vaginal walls and reduced lubrication, increasing susceptibility to infections.
Poor Hygiene Practices
Contrary to popular belief, overwashing or using harsh soaps can do more harm than good. Such practices strip the vagina of its natural protective layer, upsetting the bacterial balance. Similarly, the use of scented products, such as douches, vaginal washes, sprays, or perfumed sanitary products, can introduce irritants or allergens, making the vaginal environment vulnerable to infections. Tight synthetic clothing that traps moisture can also create a breeding ground for bacteria and yeast.
Sexual Activity
Sexual activity, particularly unprotected intercourse or having multiple sexual partners, can introduce foreign bacteria into the vaginal environment. Even semen can alter the vaginal pH, increasing the risk of bacterial infections. Additionally, certain sexually transmitted infections (STIs) like chlamydia, gonorrhea, and trichomoniasis directly lead to vaginal inflammation and infection.
Underlying Health Conditions
Chronic illnesses, such as diabetes, can significantly impact vaginal health. High blood sugar levels provide an ideal environment for yeast overgrowth, leading to recurrent yeast infections. Similarly, conditions that weaken the immune system, such as HIV or autoimmune disorders, make the body less capable of fighting off infections.
Lifestyle Factors
Stress, a poor diet, and lack of sleep can indirectly affect vaginal health by weakening the immune system. Diets low in probiotics and fibre, but high in sugar, encourage the growth of harmful bacteria and yeast. Other lifestyle factors, such as smoking or frequent hot tub use, can also increase susceptibility to infections.
Symptoms of Vaginal Infections

Identifying the symptoms of vaginal infections early is essential for effective treatment and preventing complications. The symptoms can vary depending on the type of infection, but common indicators include:
Unusual Discharge
Changes in the colour, texture, or smell of vaginal discharge are key signs of infection. For example:
Bacterial Vaginosis: Thin, greyish-white discharge with a strong fishy odour.
Yeast Infections: Thick, white, cottage cheese-like discharge, often odourless.
Trichomoniasis: Frothy, greenish-yellow discharge with an unpleasant smell.
Itching or Irritation
Persistent itching or irritation in the vaginal area is a hallmark symptom of infections, particularly yeast infections.
Burning Sensation
A burning feeling during urination or while washing the vaginal area is often reported, especially in bacterial infections and STIs.
Pain During Intercourse
Discomfort or pain during sexual activity can indicate vaginal inflammation or dryness caused by infections.
Redness and Swelling
Visible redness, swelling, or soreness around the vulva or vaginal opening is another common symptom, particularly in non-infectious irritations or allergic reactions.
Testing for Vaginal Infections

Accurate diagnosis is critical to ensuring that vaginal infections are treated effectively. Misdiagnosis can lead to the use of inappropriate medications, worsening the condition. Testing involves several methods, depending on the suspected type of infection:
Physical Examination
A doctor will conduct a visual inspection of the vaginal area, checking for redness, swelling, or abnormal discharge. They may also ask questions about symptoms, medical history, sexual activity, and hygiene practices.
Microscopic Analysis
A sample of vaginal discharge may be collected and analyzed under a microscope to identify the presence of bacteria, yeast, or other microorganisms. For example, a "clue cell" visible under a microscope confirms bacterial vaginosis, while budding yeast cells indicate a yeast infection.
pH Testing
A vaginal pH test can provide valuable clues about the type of infection. A pH higher than 4.5 typically indicates bacterial vaginosis or trichomoniasis, while a yeast infection usually does not alter the pH.
STI Screening
For sexually active individuals with symptoms suggesting an STI, a doctor may recommend tests to detect infections like chlamydia, gonorrhoea, or trichomoniasis. This is typically done using a urine sample or a swab from the cervix or vagina.
Advanced Diagnostic Techniques
In some cases, more advanced testing methods, such as polymerase chain reaction (PCR) testing, are used to accurately detect specific pathogens.
Timely diagnosis and treatment not only alleviate symptoms but also prevent complications like pelvic inflammatory disease, infertility, or recurrent infections. If you experience any unusual symptoms, don’t hesitate to consult a doctor.
Treatment for Vaginal Infection

Treatment for vaginal infections varies based on the type of infection, ensuring that the root cause is effectively addressed:
Bacterial Vaginosis (BV)
Antibiotics: Commonly prescribed options include oral or topical medications like metronidazole or clindamycin.
Lifestyle Adjustments: Avoid douching and scented products that can disrupt the vaginal flora.
Yeast Infections
Antifungal Medications: These include oral options like fluconazole or topical creams available over the counter.
Recurrent Cases: Longer treatment plans may be recommended for frequent infections.
Sexually Transmitted Infections (STIs)
Antibiotics or Antivirals: Treatment is tailored to the specific infection, such as antibiotics for bacterial STIs or antivirals for viral infections like herpes.
Non-Infectious Vaginitis
Eliminating Irritants: Switching to hypoallergenic and fragrance-free products often resolves symptoms.
Topical Creams: Anti-inflammatory or estrogen creams may be recommended for certain cases, especially during menopause.
Timely diagnosis and adherence to prescribed treatments are crucial for effective recovery. Always consult a doctor for persistent or severe symptoms.
Prevention Strategies for Vaginal Infections

Prevention of vaginal infections lies in maintaining a healthy balance in the vaginal environment. By adopting certain lifestyle practices and being mindful of habits that might disrupt the natural flora, women can significantly reduce their risk of infections.
Here's an in-depth look at prevention strategies:
Practice Good Hygiene
Maintaining proper hygiene is essential, but it is important not to overdo it. The vagina is self-cleaning and produces natural secretions that help maintain a healthy pH balance.
Use normal water to gently clean the external genital area (vulva) and avoid soaps, scented products, or harsh cleansers, as these can strip away natural protective oils and disturb the microbiome.
After using the restroom, always wipe from front to back to prevent transferring bacteria from the anal area to the vagina.
Wear Breathable Fabrics
Opt for cotton underwear and loose-fitting clothing to allow proper airflow and reduce moisture buildup. Synthetic fabrics and tight garments can trap heat and moisture, creating an ideal environment for bacterial and yeast overgrowth.
Change out of sweaty or wet clothes, such as gym wear or swimsuits, promptly to minimise prolonged exposure to dampness.
Maintain Safe Sexual Practices
Using condoms and dental dams during sexual activity significantly reduces the risk of sexually transmitted infections (STIs), which can cause vaginal infections.
Limiting the number of sexual partners and engaging in open communication about sexual health with partners are also vital.
Avoid sharing intimate items like towels or sex toys without proper cleaning, as they can harbour harmful microorganisms.
Adopt a Healthy Diet
A well-balanced diet rich in nutrients supports overall vaginal health.
Probiotics, found in foods like yogurt, kefir, sauerkraut, and other fermented products, help maintain healthy vaginal flora by promoting the growth of beneficial bacteria.
A diet high in fibre, vitamins, and minerals boosts the immune system, while reducing sugar intake can prevent yeast overgrowth.
Staying hydrated also plays a role in maintaining mucosal health and reducing the risk of dryness and irritation.
Avoid Douching and Scented Products
Douching disrupts the natural bacterial balance in the vagina, often leading to infections such as bacterial vaginosis.
Similarly, scented tampons, pads, powders, or sprays can introduce irritants that upset the vaginal environment. Stick to unscented and hypoallergenic products, and remember that the vagina does not need artificial fragrances to stay clean or healthy.
Manage Stress Levels
Chronic stress can weaken the immune system, leaving the body less equipped to fight off infections. Incorporating stress-reducing practices, such as yoga, meditation, regular exercise, and adequate sleep, can help maintain a strong immune response and support vaginal health.
Routine Check-ups and Screenings
Regular visits to a gynaecologist or doctor are essential for early detection and management of any underlying issues. Routine screenings for STIs and Pap smears can help identify potential risks and ensure timely intervention.
Myths vs. Facts
Myth: Only sexually active women get vaginal infections.
Fact: Hormonal changes, poor hygiene, or antibiotics can cause infections in women of all ages.
Myth: Douching prevents infections.
Fact: Douching increases the risk by disrupting the vaginal microbiome.
Myth: Vaginal infections always cause significant symptoms.
Fact: Some infections may be asymptomatic, emphasising the importance of regular check-ups.
Conclusion
Vaginal infections are common but entirely manageable when approached with the right knowledge and care. Understanding the factors that contribute to these infections, recognizing symptoms early, and adopting preventive measures are essential steps for maintaining optimal vaginal health. Practising proper hygiene, embracing healthy lifestyle habits, and engaging in safe sexual practices empower women to take charge of their well-being.
If symptoms of a vaginal infection arise, seeking prompt medical advice ensures accurate diagnosis and effective treatment.
Frequently Asked Questions
Can untreated vaginal infections lead to complications?
Yes, untreated infections can cause pelvic inflammatory disease, fertility issues, or recurrent infections.
Are natural remedies effective for vaginal infections?
While natural remedies like consuming more probiotics may help restore balance, they cannot replace medical treatments.
How often should I get tested for vaginal infections?
It depends on your symptoms and risk factors. Consult a doctor for personalised advice.
Can probiotics prevent vaginal infections?
Probiotics can support healthy bacteria levels and may reduce the risk of infections, but they are not a substitute for medical care.
Important
This blog, including its text, images, and infographics, is for educational purposes only and not a substitute for professional medical advice. For personalized advice, always consult a doctor.
Further Reading
For more details on this or related topics, refer to the papers listed in references below, or check out the other blogs on our website dulycare.in.
References
US Centers for Disease and Control. Vulvovaginal Candidiasis (VVC). Accessed on 24 January 2025. https://www.cdc.gov/std/treatment-guidelines/candidiasis.htm
'US Centers for Disease and Control. About Bacterial Vaginosis (BV). Accessed on 24 January 2025. https://www.cdc.gov/std/treatment-guidelines/candidiasis.htm
StatPearls. Vaginitis. Accessed on 28 January 2025. https://www.ncbi.nlm.nih.gov/books/NBK470302/
Clinical Infectious Disease. Diagnosis and Treatment of Vaginal Discharge Syndromes in Community Practice Settings. 2021. https://pubmed.ncbi.nlm.nih.gov/32350529/




Comments